
By Macy Meinhardt, Voice & Viewpoint Staff Writer
Megaphone in hand, Dr. Latisa S. Carson was among the crowd of health care providers on March 19th, 2024 who marched down to Chula Vista City Hall in protest of the closure of one of two total birthing units in South Bay–Scripps Mercy Chula Vista. “No closure, no fear! Labor, delivery, keep it here!” they shouted.
Dr. Carson admits that she has never been a boots on the ground type of activist before, “at least not on this level.” However, in the name of accessible birthing access for minorities; marching down to city hall was part of a movement to take a stand not just for the women of San Diego, but the entire state of California.
It is moments like these that serve as a poignant example of where Dr. Carson’s expertise and dedication lies within the intersection of politics and minority health advocacy.
Fielding Representation
Amid the startling statistics on Black female mortality rates, lack of access to a provider, and other socioeconomic disparities that impact pregnancy, Dr. Carson is on the front lines in pursuing wraparound equity for her patients and the industry as a whole.
Raised in Southeastern San Diego, Dr. Carson is the only female African American obstetrician-gynecologist in solo private practice in San Diego County.
Disparities in Black maternal health are tied to many factors, and one of them is quality of care. Medical researches at Mount Sinai University have found that minority women deliver in lower quality hospitals with higher maternal morbidity than whites. Using national data, the team found that 75% of black deliveries in the United States occurred in a quarter of hospitals, whereas only 18% of whites delivered in those same hospitals.
Therefore, the impact of having quality care, representation and a culturally inclusive clinical environment in the medical field is crucial for patients. It boosts physician-patient communication and trust, adherence to medical advice, follow-up rates, and therapeutic success.
Carson is noting some progress in regards to representation. In comparison to other specialists, studies show that OB-GYNS had the highest proportion of underrepresented minorities (combined, 18.4%), especially Black (11.1%) and Hispanic (6.7%) physicians, by the American College of Obstetricians and Gynecologists.
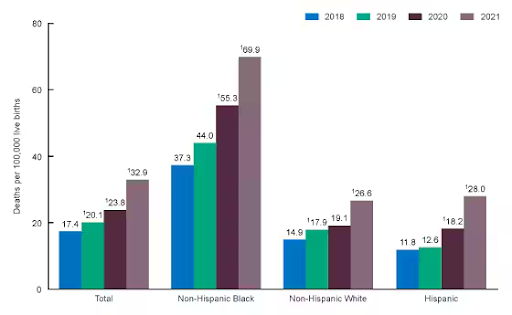
Throughout her 25-plus year journey through the reproductive industry, Dr. Carson, laments however, that in regards to actual progress for African American maternal health disparities are still glaring. Black women are three times more likely to die from a pregnancy-related cause than White women. Based on findings from the Centers for Disease Control and Prevention, Black maternal death rates jumped from 37 per 100,000 people in 2018 to 70 per 100,000 in 2021.
Misunderstood, Culturally
Dr. Carson says this disparity is tied to many complicated factors but, overall, points to how African Americans have historically been treated in the medical system.
| “I think, culturally we’re misunderstood. As far as how we say things or the way that we say things, some people misinterpret what we’re saying, and maybe they’re not able to assess us as well [as other patients].” |
Subsequently, cultural misunderstanding fuels factors such as mistrust in medical environments or the absence of culturally sensitive healthcare providers, leading to lack of preventive care.
“If you haven’t gone to the doctor, if you haven’t done preventive things, a lot of times when you come to the hospital, you’re really ill,” said Dr. Carson
In regards to maternal mortality rates, the CDC finds that most are indeed preventable; 4 out of 5 times; an 80% rate.
Barriers to Birthing Access
Manageable access to delivery services is another area Dr. Carson advocates for within her field of work. It is reported that within the past decade over 200 delivery units have closed throughout the country, mostly in urban areas that service women of color, as well as rural areas servicing Native American women. Following the recent announcement of the closure of the birthing unit at Scripps Mercy Chula Vista Hospital, Dr. Carson joined the picket line to protest against this decision.

This facility in particular serves lower income, Hispanic, and infants of color extending from Chula Vista to South Bay border cities, according to Carson. The closure is a part of a consolidation agreement to shift services to Scripps Mercy maternity campus in Hillcrest, about 1. 5 hours away from the San Diego-Mexico border, based on a public notice statement put out by Scripps.
Furthermore, Scripps says that due to continued high demand for emergency medical-surgical and cardiac services, inpatient beds at Scripps Mercy Chula Vista are currently occupied beyond full licensed capacity.” Whereas in the OB units “only half the beds are in use.”
Yet, Dr. Carson says it signifies the “devaluing of the care of women, and devaluing obstetrical services in a hospital because it doesn’t make them the money that the other departments make them.”
A circulating petition signed by Carson and a thousand other advocates details their opposition–citing that the closure will exacerbate birthing disparities, and create transportation issues, especially for mothers who rely on public transportation to get from the South Bay to Downtown.
While the initiative to keep the birthing unit open at Chula Vista was unsuccessful, it did set the tone to require more notice and due diligence before the hospitals decided to close a birthing unit.
“What we will be able to do in the future is to make it more difficult for hospitals to close their OB units without giving up a notice to the public, for the California Department of Public Health to actually come and do an investigation on to how it would impact the community if that hospital unit will be closed.”
“I’m hopeful on that part. That this will make something bigger and greater for the whole state of California and not just the local South Bay Area” said Dr. Carson.
Reducing black maternal mortality involves a multi-tiered approach involving the patient, provider and public health policy. Providers like Carson may come few and far between, however her impact has touched thousands in the southeastern community.




