By Blake Farmer, Word In Black
Medical equipment is still strewn around the house of Rick Lucas, 62, nearly two years after he came home from the hospital. He picks up a spirometer, a device that measures lung capacity, and takes a deep breath — though not as deep as he’d like.
Still, Lucas has come a long way for someone who spent more than three months on a ventilator because of COVID-19.
“I’m almost normal now,” he said. “I was thrilled when I could walk to the mailbox. Now we’re walking all over town.”
Dozens of major medical centers have established specialized COVID clinics around the country. A crowdsourced project counted more than 400. But there’s no standard protocol for treating long COVID. And experts are casting a wide net for treatments, with few ready for formal clinical trials.
It’s not clear just how many people have suffered from symptoms of long COVID. Estimates vary widely from study to study — often because the definition of long COVID itself varies. But the more conservative estimates still count millions of people with this condition. For some, the lingering symptoms are worse than the initial bout of COVID. Others, like Lucas, were on death’s door and experienced a roller-coaster recovery, much worse than expected, even after a long hospitalization.
Symptoms vary widely. Lucas had brain fog, fatigue, and depression. He’d start getting his energy back, then go try light yardwork and end up in the hospital with pneumonia.
It wasn’t clear which ailments stemmed from being on a ventilator so long and which signaled the mysterious condition called long COVID.
“I was wanting to go to work four months after I got home,” Rick said over the laughter of his wife and primary caregiver, Cinde.
“I said, ‘You know what, just get up and go. You can’t drive. You can’t walk. But go in for an interview. Let’s see how that works,’” Cinde recalled.
Rick did start working earlier this year, taking short-term assignments in his old field as a nursing home administrator. But he’s still on partial disability.
Why has Rick mostly recovered while so many haven’t shaken the symptoms, even years later?
“There is absolutely nothing anywhere that’s clear about long COVID,” said Dr. Steven Deeks, an infectious disease specialist at the University of California-San Francisco. “We have a guess at how frequently it happens. But right now, everyone’s in a data-free zone.”
Researchers like Deeks are trying to establish the condition’s underlying causes. Some of the theories include inflammation, autoimmunity, so-called microclots, and bits of the virus left in the body. Deeks said institutions need more money to create regional centers of excellence to bring together physicians from various specialties to treat patients and research therapies.
Patients say they are desperate and willing to try anything to feel normal again. And often they post personal anecdotes online.
“I’m following this stuff on social media, looking for a home run,” Deeks said.
The National Institutes of Health promises big advances soon through the RECOVER Initiative, involving thousands of patients and hundreds of researchers.
“Given the widespread and diverse impact the virus has on the human body, it is unlikely that there will be one cure, one treatment,” Dr. Gary Gibbons, director of the National Heart, Lung, and Blood Institute, told NPR. “It is important that we help find solutions for everyone. This is why there will be multiple clinical trials over the coming months.”
Meanwhile, tension is building in the medical community over what appears to be a grab-bag approach in treating long COVID ahead of big clinical trials. Some clinicians hesitate to try therapies before they’re supported by research.
Dr. Kristin Englund, who oversees more than 2,000 long COVID patients at the Cleveland Clinic, said a bunch of one-patient experiments could muddy the waters for research. She said she encouraged her team to stick with “evidence-based medicine.”
“I’d rather not be just kind of one-off trying things with people, because we really do need to get more data and evidence-based data,” she said. “We need to try to put things in some sort of a protocol moving forward.”
It’s not that she lacks urgency. Englund experienced her own long COVID symptoms. She felt terrible for months after getting sick in 2020, “literally taking naps on the floor of my office in the afternoon,” she said.
More than anything, she said, these long COVID clinics need to validate patients’ experiences with their illness and give them hope. She tries to stick with proven therapies.
For example, some patients with long COVID develop POTS — a syndrome that causes them to get dizzy and their heart to race when they stand up. Englund knows how to treat those symptoms. With other patients, it’s not as straightforward. Her long COVID clinic focuses on diet, sleep, meditation, and slowly increasing activity.
But other doctors are willing to throw all sorts of treatments at the wall to see what might stick.
At the Lucas house in Tennessee, the kitchen counter can barely contain the pill bottles of supplements and prescriptions. One is a drug for memory. “We discovered his memory was worse [after taking it],” Cinde said.
Other treatments, however, seemed to have helped. Cinde asked their doctor about her husband possibly taking testosterone to boost his energy, and, after doing research, the doctor agreed to give it a shot.
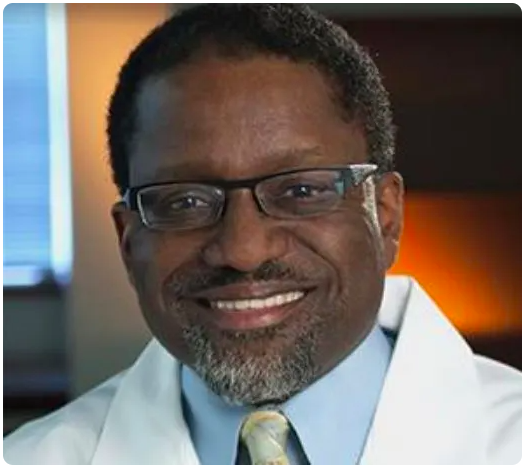
“People like myself are getting a little bit out over my skis, looking for things that I can try,” said Dr. Stephen Heyman, a pulmonologist who treats Rick Lucas at the long COVID clinic at Ascension Saint Thomas in Nashville.
He’s trying medications seen as promising in treating addiction and combinations of drugs used for cholesterol and blood clots. And he has considered becoming a bit of a guinea pig himself.
Heyman has been up and down with his own long COVID. At one point, he thought he was past the memory lapses and breathing trouble, then he caught the virus a second time and feels more fatigued than ever.
“I don’t think I can wait for somebody to tell me what I need to do,” he said. “I’m going to have to use my expertise to try and find out why I don’t feel well.”



