By LAURA UNGAR, AP Science Writer
Regulators on Friday approved two gene therapies for sickle cell disease that
doctors hope can cure the painful, inherited blood disorder that afflicts mostly
Black people in the U.S.
The Food and Drug Administration said the one-time treatments can be used for
patients 12 and older with severe forms of the disease. One, made by Vertex
Pharmaceuticals and CRISPR Therapeutics, is the first approved therapy based on
CRISPR, the gene editing tool that won its inventors the Nobel Prize in 2020.
The other is made by Bluebird Bio and works differently.
“Sickle cell disease is a rare, debilitating and life-threatening blood disorder
with significant unmet need,” the FDA`s Dr. Nicole Verdun said in a statement
announcing the approvals. “We are excited to advance the field especially for
individuals whose lives have been severely disrupted by the disease.“
The two gene therapies are the first approved in the U.S. for sickle cell. The
FDA has previously OK`d 15 gene therapies for other conditions. Some have list
prices in the millions of dollars, and the sickle cell therapies will too.
In the U.S., an estimated 100,000 people have sickle cell and about a fifth of
them have the severe form. Sickle cell is most common among Black people and 1
in 365 Black babies are born with the disease nationally. Scientists believe
being a carrier of the sickle cell trait helps protect against severe malaria,
so the disease occurs more often in mosquito-prone regions such as Africa or in
people whose ancestors lived in those places.
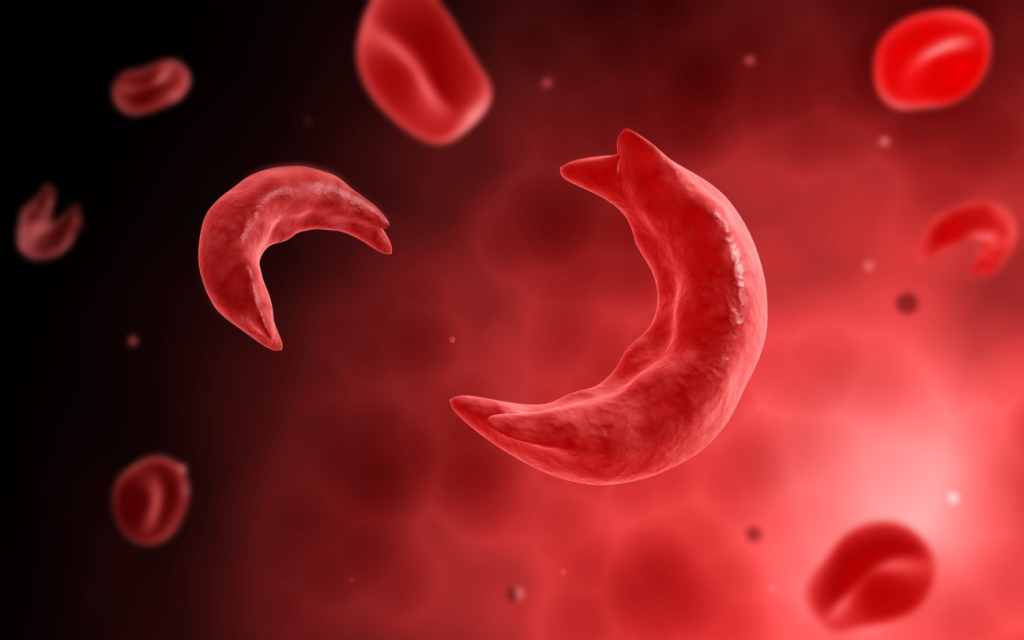
The disease affects hemoglobin, the protein in red blood cells that carries
oxygen. A genetic mutation causes the cells to become sickle or crescent-shaped,
which can block blood flow, causing excruciating pain, organ damage, stroke and
other problems.
Current treatments include medications and blood transfusions. The only
permanent solution is a bone marrow transplant, which must come from a closely
matched donor and brings a risk of rejection.
No donor is required for the gene therapies, which permanently change DNA in the
patient’s blood cells. The goal of the Vertex therapy, called Casgevy, is to
help the body go back to producing a fetal form of hemoglobin that’s present at
birth __ it’s the adult form that’s defective in people with sickle cell disease.
CRISPR is used to knock out a gene in stem cells collected from the patient.
Bluebird’s treatment, called Lyfgenia, aims to add copies of a modified gene,
which helps red blood cells produce “anti-sickling” hemoglobin that prevents or
reverses misshapen cells.
When patients get the treatments, stem cells are removed from their blood and
sent to a lab. Before getting the altered cells back, they must undergo
chemotherapy. The process requires at least two hospitalizations, one lasting
four to six weeks.
Still, many patients say they’d consider gene therapy given the seriousness of
the disease.
Jalen Matthews of Louisville, Kentucky, was diagnosed with sickle cell at birth
and had her first pain episode at age 9. Three years later, the disease led to a
spinal cord stroke that left her with some paralysis in her left arm and leg.
“I had to learn how to walk again, feed myself, clothe myself, basically learn
how to do everything all over again,” said Matthews, now 26.
Today, she keeps her sickle cell at bay with transfusions every two months or so,
with five units of her blood replaced with healthy cells. She said gene therapy
could be a better option and she plans to ask her doctor about it.
“This one-time kind of cure is very much needed,” said Matthews.
The FDA’s approval is the first for Bluebird’s treatment; Vertex has been
previously authorized in Britain and Bahrain.
Studies testing the therapies suggest they work well. Of 31 people treated in
the pivotal Vertex study with sufficient follow-up, 29 were free of pain crises
for at least a year. In the Bluebird study, 28 of 32 patients had no severe pain
or organ damage between six and 18 months after the therapy.
But doctors point out there are possible side effects and the long-term outcomes
are unknown. For both, the necessary chemotherapy comes with risks such as
infertility, hair loss and vulnerability to serious infection.
With the Bluebird therapy, blood cancer has occurred, so the FDA said the label
will include a “black box warning” about that risk. With the Vertex therapy,
some scientists worry that CRISPR brings the possibility of “off-target effects,
” which are unexpected changes to a person’s genome.
“It’s important to be cautious and to be optimistic about this therapy, but also
know that there’s still not a ton of experience with it,” said Dr. Benjamin
Watkins, director of the pediatric stem cell and cell therapy program at
Children’s Hospital New Orleans.
Doctors said they don’t expect every medical center to offer the gene therapies
because they require so much equipment and coordination between medical
specialists. They also don’t expect lots of people to seek them right away.
Watkins said some may want to wait until more people get the treatments.
Experts also warned that cost could be a hurdle. The list price for Bluebird Bio
is $3.1 million and for Vertex, $2.2 million. What patients might pay will
depend on insurance coverage and other factors. To help cover the cost, the U.S.
Centers for Medicare and Medicaid Services announced a plan that aims to
establish partnerships with state Medicaid agencies and drug companies.
But eventually, gene therapy “could be transformative and really change the
landscape of sickle cell disease,” said Dr. Monica Bhatia, who treats children
with the disease at NewYork-Presbyterian.
Matthews, who volunteers with The Sickle Cell Association of Kentuckiana, said
she’s hopeful the treatments will have a big impact.
“It’s a blessing,” she said. “It will really benefit all of us in the sickle
cell community.”



